Myopia Management: A Deeper Look
Myopia management is a revolutionary movement in eyecare that demonstrates a proven form of slowing down the progression of nearsightedness. In April of 2021, the World Council of Optometry recommended that myopia management be considered a “Standard” in eye care.
Visit our home page DeliverContacts.com and switch to big savings on your lenses. Easily prescription renewals, no games or gimmicks. We sell Acuvue, Alcon, Bausch&Lomb, and CooperVision at the Internets consistently lowest prices.
Introduction to Myopia Management: A New Standard in Eyecare
Myopia management is a revolutionary movement in eyecare that demonstrates a proven form of slowing down the progression of nearsightedness. In April of 2021, the World Council of Optometry recommended that myopia management be considered a “Standard” in eye care.
But before we dive into the treatment itself, let’s discuss what we have known all along.
Understanding Myopia: How Light Focus Affects Vision
Light is supposed to enter the eye through the pupil and focus at a point in the back of the eye in the center of the macula of the retina at a precise point called the fovea for the most detailed and precise visual perceptions of the eye. With myopia (aka: nearsightedness), the eye tends to grow in length as a growing body develops causing the actual focal point of light to fall short of the fovea. The further the point of focus separates from the fovea, the blurrier that objects become at greater distances. – Hence, the term “nearsighted” is used to reference myopia… say what you CAN see… “I HAVE near sight (not far sight), so I am considered nearsighted.” – Until myopia management, the only thing we would routinely do is chase the growth by moving the focal point back to the fovea with glasses or contact lenses. We thought that genetics was in complete control of the growth and elongation of the eye and there was nothing we could do about it.
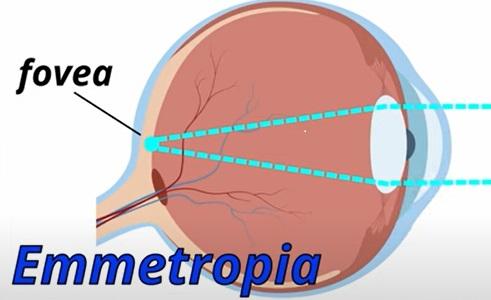
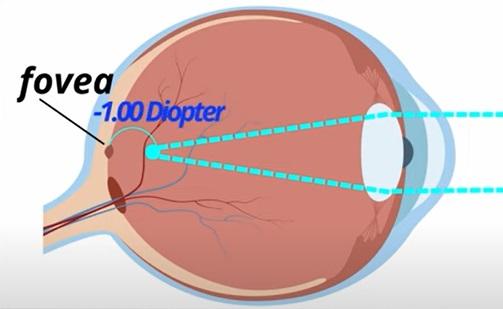
- When an eye has “perfect focus,” light focuses directly on the fovea (left image). This state of perfect focus without correction needed is called Emmetropia.
- When the eye grows in length, leaving the focal point in front of the fovea, vision will become blurred. This state of imperfect focus is called Myopia.
- In this example, the myopia requires -1.00 Diopters of focus correction to see clearly again.
The Evolution of Myopia Management: From Skepticism to Acceptance
Over the last few decades, discussion surfaced about methods of slowing the lengthening of the eye, therefore also slowing myopic progression eye growth. Early data seemed inconsistent and correlative rather than defined by deep research. Being thinly supported with data, considering implementation of myopia management in the early stages of development seemed to be a practice that preyed upon the concerns of loving parents who are willing to do and give anything for their children. Hence, many doctors distanced themselves from its practice and developed bad feelings toward its design. Every ocular industry claim continuously needs to be sorted into “relevant” or “gimmick”, and no good doctor has any desire to betray their patient’s trust by chasing every fad in care. And so, to myself and many of my colleagues, myopia management sounded ridiculous and we wanted nothing to do with it when strange and weakly supported claims were surfacing.
But regardless of my viewpoint, great minds in ocular care continued to test, observe, and formulate results and concepts that eventually lead to a recognized pattern of control over the visually disruptive growth of the developing eye. Ultimately, data overwhelmingly suggested that treatment during the progressing years of myopia with new designs and uses of contacts, glasses, or eyedrops can limit the endpoint of ocular growth. So, whether I was on board or not, myopia management had demonstrated itself as a genuine form of optometric and ophthalmologic intervention.
The movement of support for myopia management is now undeniable. It is a revolutionary reality. The data proves that we currently have a way to slow the progression of myopia up to 50%. Fifty percent is a lot. Therefore, no more kicking and screaming for me… I’m on board now.
A few points must be considered before electing to engage in myopia intervention practice. Though proven as a working form of myopia management, results can not be promised. It must be understood that this is a revolutionary intervention, and the methods of application are still being refined and the understanding of the best practice designs and results are still growing. Results vary. We can attempt to slow the disease based upon our current understanding, and hopefully, yield obvious successful results, but we can not promise anything. On top of that, whether successful or not, the intervention will cost extra time and money. Myopia management is not considered a part of a “routine” exam. Extra overall costs will depend upon your provider’s pricing schedule, the number of visits needed, and the mode(s) of intervention chosen. And since positive results can not be promised, refunds for unsatisfactory endpoints will not be given.
Decoding Myopia Management: Targeted Treatment for Children’s Vision Growth
Let’s now dive into what myopia management actually consists of. Simply put, myopia management is targeted treatment for growing children especially between 5-16 years old to limit the progression of myopia (nearsightedness). This is important because as bodies grow, so do eyes. Early OVERALL growth (including the cornea and optics) of the eye occurs from birth to about 5 years old. Then, after 5 years old (for the most part), the eye only changes in length (aka: axial length). When the optics can’t keep up with the elongating eye, the eye will need more dioptric power to keep up with proper focus on the fovea.
Here is an imperfect example, intended to help your understanding of how the elongation of the eye’s axial length contributes to myopia… If we know that a child’s eye is 23.5 mm in length at 5 years old, and we understand that normal growth rates of the eye will be a millimeter and a half through their growing years, then we can predict that their eye is very likely to become nearsighted, and potentially advance to what we call “HIGH MYOPIA.” High myopia not only causes excessive blur in the distance, but also increases other ocular health risks throughout the rest of the child’s life. This likely progression is predictable based on already established normative data.
Think of it this way… You know how pediatric health doctors often estimate the future height of a child by using graphs for boys and girls? The charts are definitely not perfect, but they usually can identify whether a child’s height is below, at, or above the expected range, and it gives a normative “guess” about their final adult height. Now, sometimes we can just look at mom and dad and say, “They’re both 6’5”, so I can predict that their child is likely to be tall as well,” and we don’t even need the charts. Their child will likely follow the plotted course on the normative data chart that indicates that the child will be tall as well.
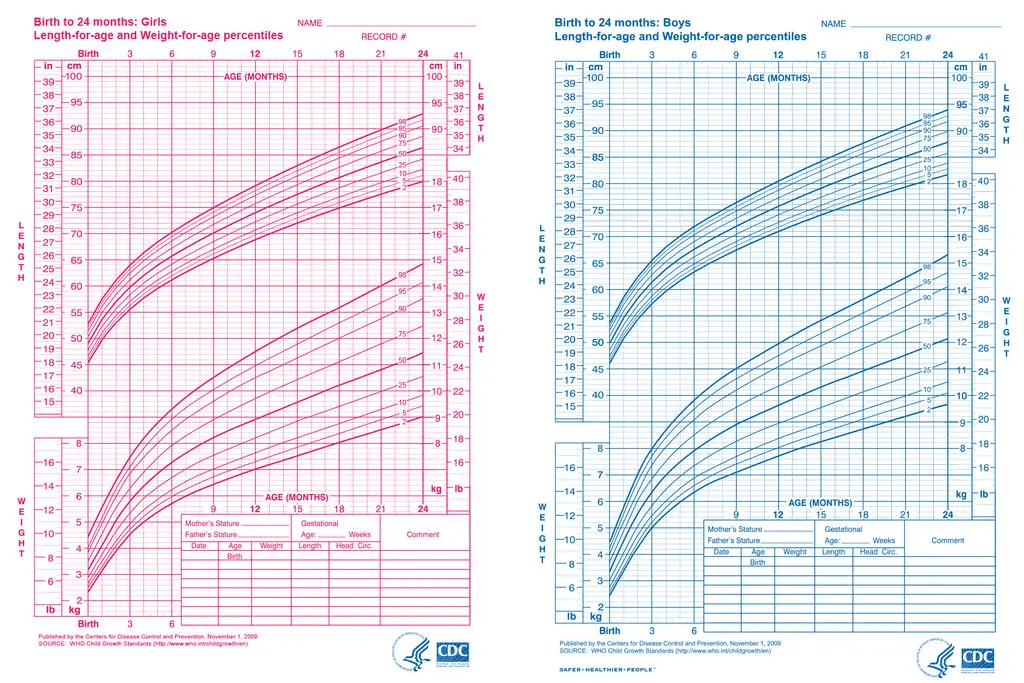
Image from: https://www.cdc.gov/growthcharts/clinical_charts.htm#print
And it’s the same way with myopia… if mom and dad are both highly nearsighted, we can predict that their child is also likely to be highly nearsighted, right? We also have similar charts for boys and girls that we can plot age and the axial length of the growing eye in a similar fashion, and give a strong estimate on where the eye will grow. And so, if we combine the charts with the parent Rx information, and recognize the likelihood of myopic progression due to axial length, then a strong case can be built to try to limit the extent of myopic development that occurs in a child’s progressing eye.
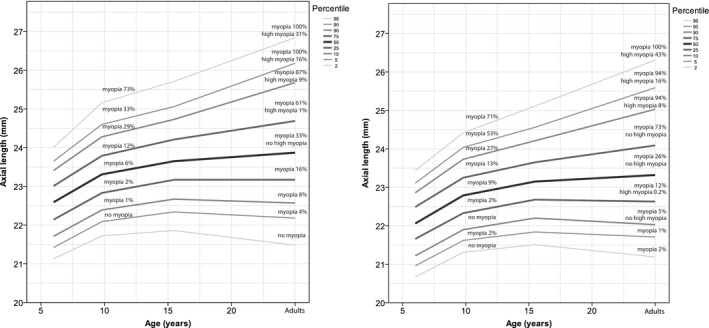
Image from: Acta Ophthalmol. 2018 May; 96(3): 301–309.
Predicting and Managing Myopia in Children: A New Approach
The implementation of MYOPIA MANAGEMENT is intended to limit the amount of axial length and so limit the amount of myopia that occurs for children who are expected to have myopia. We can measure axial length with various simple to use, noninvasive biometric devices. Measurements will yield that not every child needs myopia management. So the question becomes, “Which kids need intervention?” To answer this, we must consider standard visual performances with certain levels of myopia represented in dioptric power.
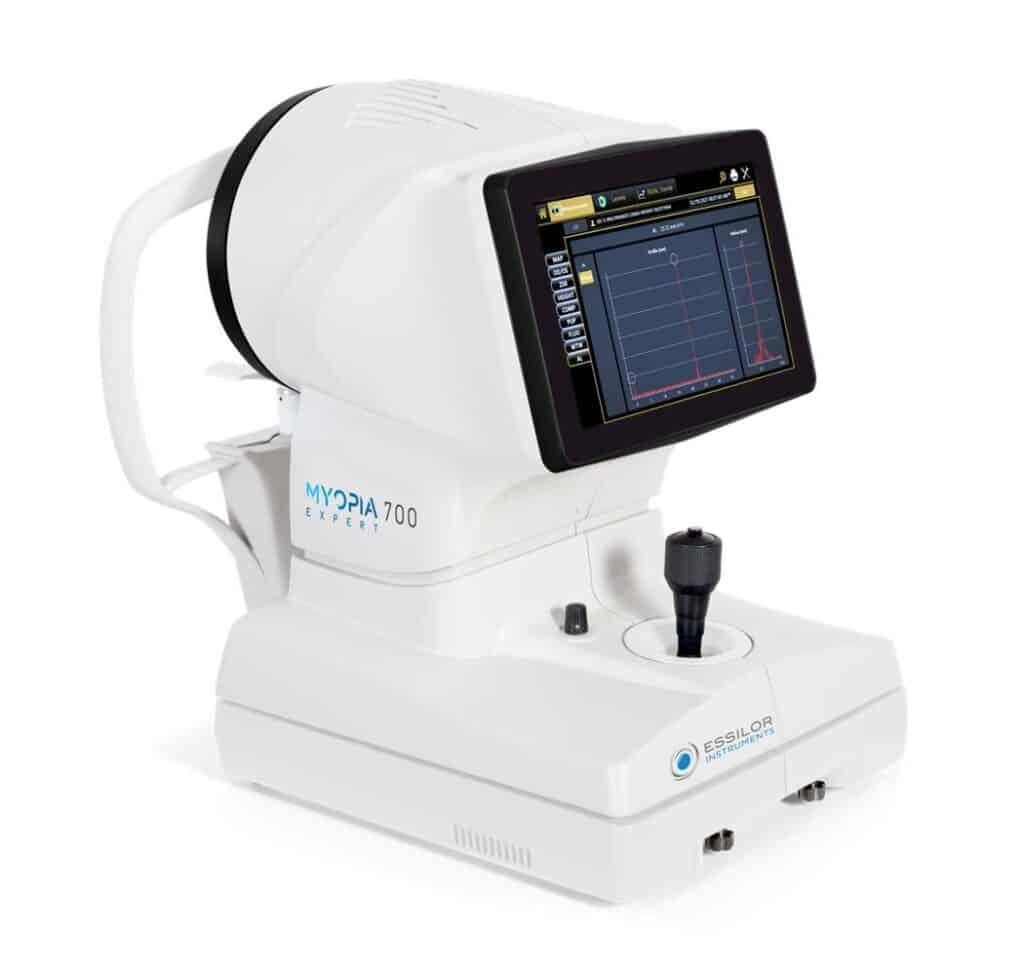
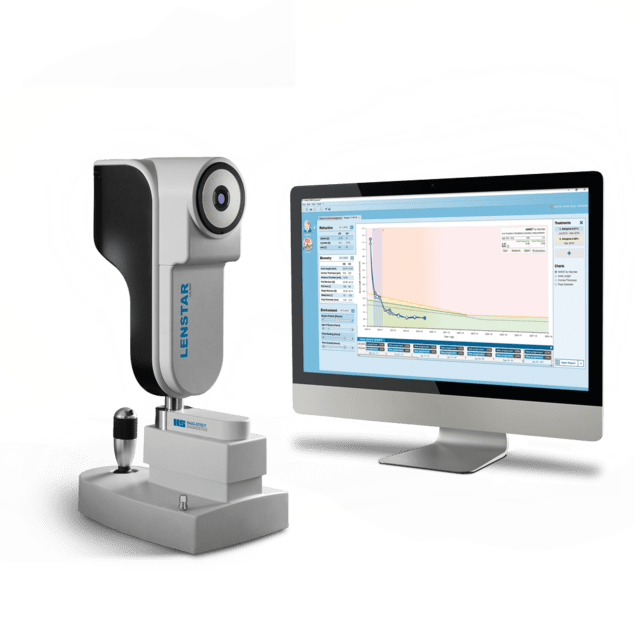
Examples of biometry devices often measuring axial length:
The unit “diopter” is represented with the letter “D”. The lower the dioptric power, the lesser the gap that light is out-of-focus from the fovea. The higher the dioptric power, the greater that light is out-of-focus. As light becomes focused off of the fovea, the distance that light is needed to be moved to refocus on the fovea represented by the diopter (D) power. Here are some dioptric power measurements to give perspective with a comparison to expected visual acuity (VA).
- 0.00 D = light is focused on the fovea; vision is as good as it can be; VA = 20/20
- -0.50 D = barely noticeable vision affects, especially noticed at night; VA = 20/25
- -1.00 D = vision becomes very bothersome for typical daytime vision; VA = 20/40
- -1.50 D = vision affected to become not legal to drive without glasses; VA = 20/70
- -3.00 D = vision severely blurred; eye health risks start to climb; VA = 20/300
- -6.00 D = vision even blurrier; and eye health risks sky rocket; VA = 20/600
Visual acuity compares a patient standing at 20 feet from a sign and can barely perceive it, and compares them to a “person with normal vision”. Example: VA = 20/70 means that the patient is at 20 feet and can barely read the sign, while a “person with normal vision” can stand at 70 feet and barely read the same sign.
Since myopia management can reduce myopia progression as much as 50%, then a -6.00D child’s destined Rx may potentially be reduced a -3.00D. Or a -3.00D may only end up -1.50D. Or a -1.00D may end up as a -0.50D. The extent of benefit and reduction is relative to each individual. Overall, doctors and parents may each have different perspectives on why to manage, but the more the parent understands, the better they can consider their decision as whether to treat or not.
As eye doctors, our greatest concern is limiting the progression of myopia to reduce the risk for a lifetime of sight threatening vision issues. As the eye grows during the formative years, the retina does not grow with it. Instead, the retina is stretched along with the growing eye. When the retina is stretched, there is a greater risk for thinning, degeneration, and tearing. Lifetime diseases of the eye associated with this early stretching include retinal detachment and maculopathy which increase the chance for retinal bleeding and the need for injections, lasers, and surgery intervention to limit sight loss. Therefore, limiting long term pathological myopia is the ultimate desired effect for doctors. And the greater the axial length, the greater the pathological myopia risk. On top of that, the greater axial length, the greater association with increased dioptric power. That’s why -6.00D and above is considered HIGH RISK… it is tightly associated with excessive axial length.
As parents, you may also highly consider other quality of life factors associated with myopia. Such concerns are: How well can my child see without glasses or contacts? Can they function to recognize the world around them? Can they see the leaves on trees? Can they see faces or expressions? How will the vision limitation affect learning? Can they see the board? How will this affect sports? Can they wear glasses comfortably with a helmet? Are contact lenses an option? Will they be legal to drive without glasses? How thick will the glasses be? How much extra will higher index lenses (to thin the lenses) cost over a lifetime? How will this affect self image? And last but not least, “How much will this cost?” and “How long do we have to do this?” These are all questions for the family to consider along with the increased risk for pathological myopia before proceeding with myopia management.
Myopia Management Techniques: Optical and Medicinal Interventions
There are various ways to implement myopia management. The simplest form of management includes behavior modifications. For example, there is more research suggesting that outdoor sunlight exposure with non-reading activity may reduce the progression of myopia, so 2 hours outdoors per day is recommended. It is also suggested that at risk eyes decrease duration of near activity to 30 minute intervals, and keep work distances greater than 12”. Also, make sure children are wearing their proper correction. Not wearing the full correction seems to amplify growth as well.
Beyond the simple behavior modifications, there are also ways to limit growth optically. Remember how light is supposed to focus on the fovea for clarity? Well, apparently, studies are recognizing that the focus away from the fovea, that focuses behind the peripheral retina (called Hyperopic Defocus), is directly contributing to the increased growth of the eye. The eye is trying to keep up with this peripheral focus. CRAZY stuff, but apparently real, because the intervention methods work. So, let’s first discuss the optical methods of myopic management.
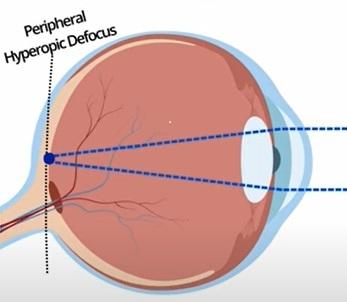
Hyperopic Defocus occurs away from the fovea. Notice that when light properly focuses on the fovea (the blue point imaged in the back of the eye), the retina away from the fovea is not focused. When light focuses behind the retina, it is considered “hyperopia”. Therefore, this peripheral area of unfocused hyperopia is considered “Hyperopic Defocus”.
Innovative Contact Lens Solutions for Myopia Control
Contact lenses provide the current best optical method to support myopia management by addressing the peripheral hyperopic defocus with dual focus lenses. Remember that all light enters through the pupil of the eye to reach the retina. The very center of a myopia management contact lens is designed to focus that very important light on the fovea for detailed visual acuity, but the surrounding zones incorporate a different power, intended to reduce the hyperopic defocus and thus reduce the stimulus for axial length growth.
As of today (January 1st, 2024), the only FDA approved soft contact lens approved for management of myopia in the US is CooperVision’s MiSight, a 1-day disposable lens (the lens is worn for one day, and then discarded). It’s approved for use between the ages of 8-12 years old, but that doesn’t mean that it can not be used for other ages. This lens utilizes concentric rings intended to turn the hyperopic defocus plane into a myopic defocus plane, and has shown to reduce the axial length growth by 52% according to a three year study (Chamberlain P, et al. A 3-Year Randomized Clinical Trial of MiSight® Lenses for Myopia Control. Optom Vis Sci. 2019;96(8):556-7. 2. Tideman JW, et al. Association of Axial Length With Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016;134(12):1355-63). CooperVision has another lens that has been around for a long time called the Biofinity +2.50 D (D represents “Dominant eye” in this lens). This multifocal designed lens for adults has been used because it has a traditional center optic zone for foveal focus, and a peripheral zone with a +2.50 add power (which acts to reduce the peripheral defocus), but it does not demonstrate the same success rates as the MiSight.
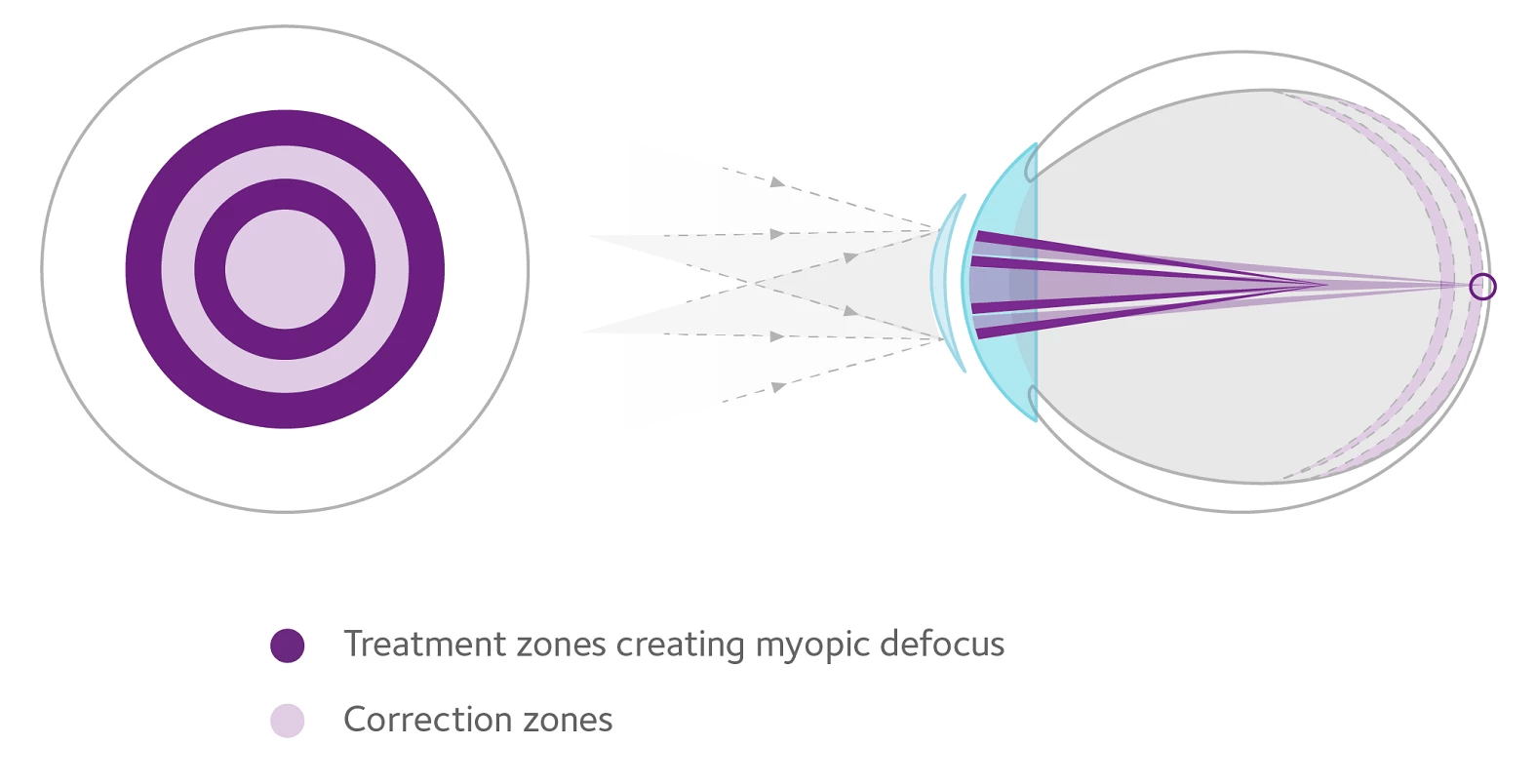
MiSight contact lens design: Image from https://coopervision.com/practitioner/our-products/misight-1-day/misight-1-day
Johnson & Johnson has a soft contact lens design of their own called the ACUVUE ABILITI 1-day lens. Though it is not utilized in the US right now, it is earning excitement from its exceptional design options. Firstly, the Abiliti 1-day is made of senofilcon A, a silicone hydrogel material that is currently utilized in the Oasys brand lenses and is a much more oxygen permeable material than the MiSIght lens material, omafilcon A. Secondly, different designs of “Ring Boost” (which is another design of center fovea optics with peripheral defocus zones) are available in both an EE (Enhanced Efficiency) design and an EV (Enhanced Vision) design. It appears that each design has its benefits. The EE design has more peripheral defocus effect, but the central optics are slightly limited, while the EV design has a wider foveal focus zone, with lesser peripheral defocus effect. It appears that the EE has the greater effect of limiting axial growth, but trials are in place to determine the efficiency of each and the comparison between them. This lens should not be confused with the similarly named ACUVUE ABILITI Overnight lenses, which are used as an orthokeratology lens.

Abiliti 1-Day Soft Lens Image from: https://www.seeyourabiliti.com/sg/professionals/abiliti-portfolio/abiliti-1-day
Use of an orthokeratology lens (aka: “ortho-K”) has been a longstanding optometric practice of wearing rigid gas permeable lenses (much stiffer than than soft lenses) to alter the shape of the cornea during sleep so that, when a person with myopia wakes, they can see without glasses until the effect wears off. This nighttime wear lens presses down on the center of the cornea and steepens the peripheral cornea, essentially warping the corneal optics to favor a more foveal optically corrected state. The concern with this method is that the cornea is being intentionally warped by design, and is a reason why many eye doctors prefer not to partake in this procedure. Newer technological designs have made ortho-K much simpler over the years, but it still requires artistic experience and a commitment to the process from the patients as well. For many doctors who have utilized ortho-K over the years, they have correlated reduced myopic progression with ortho-K treatments, but the link is much harder to quantify due to the fact that the axial length is being manipulated with the ortho-K procedure.
Orthokeratology and Spectacle Lenses: Alternative Myopia Management Methods
Another way to address the peripheral defocus is by using spectacle lenses. The current lens designs utilized are Highly Aspherical Lenslets (HAL), Defocus Incorporated Multiple Segments (DIMS), and Diffusion Optics Technology (DOT). Less specific designs that utilize older methods of lens designs include Executive Prismatic Bifocals (+1.50 add) and Progressive Additional Lenses (PAL’s). The greatest concern with spectacle lenses is that the optical center does not move with the eye like a contact lens does. However, my number one rule with wearing contact lenses is this, “Contacts should only be worn IN ADDITION to glasses, not INSTEAD OF glasses” for the least risk of contact lens related issues. So, if you want to go all-in with the myopia management process, then these lenses provide for the hours that contact lenses are not being worn, or for the child who will not be wearing contact lenses.
Exploring Medicinal Approaches: Atropine Eye Drops in Myopia Management
There is also a medicinal way to slow the progression of myopia. This method uses low dose Atropine eye drops. Atropine is an acetylcholine receptor blocker. It causes the iris constrictor muscles, the circular muscles of our pupil to relax, and reduces the ciliary muscle focus. Initially, it was thought that it was the reduction of the mechanical constricting effect of the ciliary muscles that reduced the axial length growth, but the effect was not there. This mechanical mechanism of action is not the cause. So, in reality, we do not fully understand how low dose atropine slows myopic progression. However, since Atropine has been observed for so many years, the resultant effect on myopia is greatly understood.

Three dose options of Atropine for Myopia Management Image from: https://www.atropine.com/prescribe.html
There are three doses of Atropine that may be used in myopia management: 0.05%, 0.025%, and 0.01%. The highest dose, 0.05% has the greatest effect on reducing axial growth, but also has the greatest effect on increasing light sensitivity and disrupting the focusing system of the eye. Light sensitivity can be offset by photo-changing lenses and the reduced focus can be offset with near lenses, but is it worth it? Eye doctors will often push for the higher dose because there is a greater demonstration of myopia management with the higher dose form, but the parent needs to consider the child’s concerns as well. To what extent will the dilation and photophobia effect limit the individual child? Dosage needs to be considered by parents with the doctors when deciding upon a plan. Besides, there are lower doses that also demonstrate myopia management with lesser vision effects, but at the cost of potential lesser management. If conflicted, the middle ground dose is 0.025%. If the desired effect for myopia management is not being achieved, then up the dose. If the light sensitivity and focus effect is too much, then reduce the dose… it’s a simplified plan, but not the expected best plan for every child.
Other interventions include red light treatments and blue light treatments. These designs have demonstrated results that can be implied to limit myopic progression, but the research in these design areas is still being accumulated.

Eyerising Myopia Management Device Repeated Low-Level Red-Light (RLRL) therapy Image from https://www.eyerisinginternational.com/the-device/
Combining Strategies for Enhanced Myopia Management
Most eye doctors that practice myopia management do not rely on one of these methods to treat their young patients, instead they are employing a combination of plans. Combinations do seem to have an additive effect on limiting growth, but not exactly like we’d hope. For example, if you get a 50% reduction from a contact lens, and a 30 % reduction from atropine, you shouldn’t expect an 80% overall reduction effect. But, given our growing understanding, we can definitely hope for greater myopia control by attacking from a combination of directions.
The Future of Myopia Management: A New Frontier in Eyecare
In the end though, we will likely never know exactly how much each intervention or combination of interventions will make for your specific child, but we can confidently now state that studies suggest that interventions do make a difference. The Myopia Management Movement is here to stay. It’s a new and developing frontier in eyecare that has earned its place.
Parental Decision-Making in Myopia Management: Weighing the Options
Each parent, along with their doctor, must determine the risk and reward of each optional myopia management intervention. Even though an eye doctor may press one way or another, it is still the parent’s decision in the end. Nothing is mandatory, and everything is optional. We are all currently sifting through what works and what doesn’t for each of us, but in the meantime, the kids are still growing, and the window of intervention is narrow. So right now, we have to go with what we got, and each parent must decide whether myopia intervention is right for their child or not.
Conclusion: Embracing the Myopia Management Movement
Again, this is new and revolutionary. We can expect greater understanding and better control in the upcoming years. It’s a very exciting time for eye doctors and the world. In the not so distant future, we will probably remember with disbelief the days when we couldn’t control myopia. So, keep an eye out for new and innovative updates… about this “new thing” we call myopia management.
Need Consistanly Cheap Contacts?
DeliverContacts.com always guarantees you are paying low prices, every time you buy. We will never play games with our pricing or take part in manipulative discounts. Just consistently cheap contacts, forever.
Give your box a search below and see for yourself! 100% Free shipping and returns on all products!
